By: Kyle Stafford, DPT, CSCS (Certified Strength & Conditioning Specialist)
SUMMIT Physical Therapy
Statistics
According to the American Academy of Orthopedic Surgeon’s, there are approximately 200,000 annual ACL injuries. Roughly 50% of those result in ACL reconstruction surgery and damage to other structures of the knee joint (ligaments, meniscus, cartilage).
A recent study showed that 1 in 100 high school female athletes will injure their ACL at some point. Roughly 70% of ACL injuries by female athletes are due to non-contact situations involving deceleration, planting, landing, twisting, cutting and movements requiring agility. The primary sports involving this type of stress entail soccer, basketball, football, and skiing.
Down the road, approximatelty 50-60% of these patients will show imaging/radiographic results of early osteoarthritis. Osteoarthritis is a big precursor for having a total knee replacement. You see where this trend is heading…
The neuromuscular system
The neuromuscular system is the interaction between your nervous & muscle systems. Your ACL is one of the ligaments in your knee, of which it contains “proprioceptors”. These are receptors that allow your knee to detect where it is in space, and interact with your nervous system to tell your muscles to stabilize your joint. This is crucial in sports that require agility, cutting, jumping, pivoting, etc… When you undergo surgery or sustain an injury your proprioceptors are diminished and must be re-trained to provide your knee with reactive stability. Notice I said reactive, because many times athletes have sufficient stability in a predictable environment such as practice or a rehab facility. Sports are a series of reactions, plays and events that take place where an individual must react to a unpredictable task at hand.
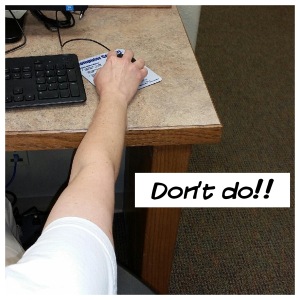
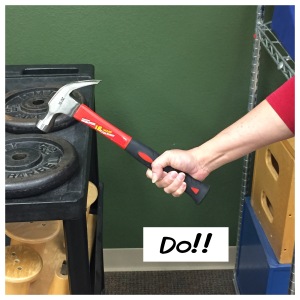
Body mechanics in running, jumping & landing
The change of direction, whether it be running, cutting/pivoting, jumping, landing, shuffling or any other movement, occurs with every player of every play. These repetitive movements place stress on the knee joint. Learning how to move in all of these movements efficiently is similar to installing the appropriate shocks & brakes on your vehicle. Athletes are larger in stature than any time in history. You would not want to head down a hill in a Ford F-350 with the shocks/brake pads of a Toyota Prius. Ignoring mechanics and trying to “strengthen only” is like heading down the hill in the same F-350 but with a truck bed full of bricks and bigger tires installed. “Use proper mechanics. The No. 1 problem in any specific sport is improper mechanics”, as stated by Dr. James Andrews in his recent STOP(sports trauma overuse program.)
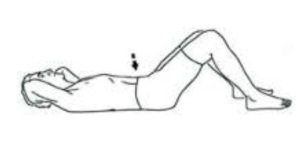
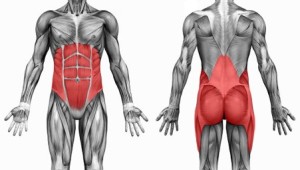
Core/lower extremity strengthening
We have all heard the term “core strength”, but understanding what entails the core is critical. Your hips/glutes, abdominals, lumbar/low back, diaphragm and oblique muscles to name a few, all serve as the central band of stability for spine & extremities. Developing core strength along with mechanics/movement patterns will help the individual move more efficiently and reduce stress on the body. Every human on the planet can benefit from core strength, and athletes must demonstrate this to a whole new level. For basketball players, we aim to develop core strength/stability in conjunction with movement or dynamic postures. Training the body to react to provide stability while moving is absolutely critical for injury prevention.
Rest & specialization
I want to inform you that modern medicine is showing that kids specializing in sports early are at a much higher risk for injury. Different sports utilize different muscle groups and movements. In the present day, kids are playing 1 sport year round without proper rest. Less than 2 months of rest per year can drastically increase your child’s chance of injury. So with that being said, I fully advocate and encourage your daughter to rest after basketball season or whatever sport they play. That does not mean or equal doing nothing. It does not mean that it has to be 2 months in a row of rest, as it can be 1-2 weeks here and there. We hate seeing adolescent patients with injuries at such a young age, when the simple solution to help is to play another sport or take a break at times.
Community change
The purpose of this document is to help inform you as parents, and communicate the aim I have to change our community sports programs to help our young athletes. Injury prevention is becoming very significant in large cities and advanced areas of sports training/medicine. It is my intent to help establish this task of helping educate parents, coaches, teams and youth organizations of the importance of injury prevention for the future leaders of our community. If you have any questions, concerns or general comments, please feel free to contact me at SUMMIT Physical Therapy.
Contact Kyle Stafford, DPT at 918.342.3800.







 7 things you didn’t know about Posture….
7 things you didn’t know about Posture….